SAVE BIFIDOBACTERIA: PROTECT GUT MICROBIOTA THANKS TO AN INNOVATIVE BIFIDOBACTERIAL STRAIN RESISTANT TO AMOXICILLIN + CLAVULANIC ACID
Antibiotics are universally recognized as a fundamental tool. These drugs are sometimes the only ones able to defeat bacterial infections and improve the health conditions of those affected. However, they are also the cause of a reduction in the number of commensal bacteria, all those bacteria that are naturally present and do not cause damage, and, conversely, can contribute to the body’s defense mechanisms, playing a crucial role for a healthy gut.
Over the course of a lifetime, the intestinal microbiota can also be frequently exposed to the use of antibiotics. Each time this determines a reduction in the bacterial populations and therefore an alteration of the microbiota ecosystem, with immediate effects, but also with long-term indirect effects on the health of the host. There are numerous and recent researches, for example, that study the relationship between early exposure to antibiotics and its impact on the composition of the microbiota and associated health conditions in children.
Unfortunately, the use of the most common probiotics during antibiotic therapy is not a good option to buffer the decline in good bacteria, since the products on the market often do not have characteristics that allow them to resist the activity of the antibiotics used, as they also are overwhelmed by the bactericidal action of these drugs.
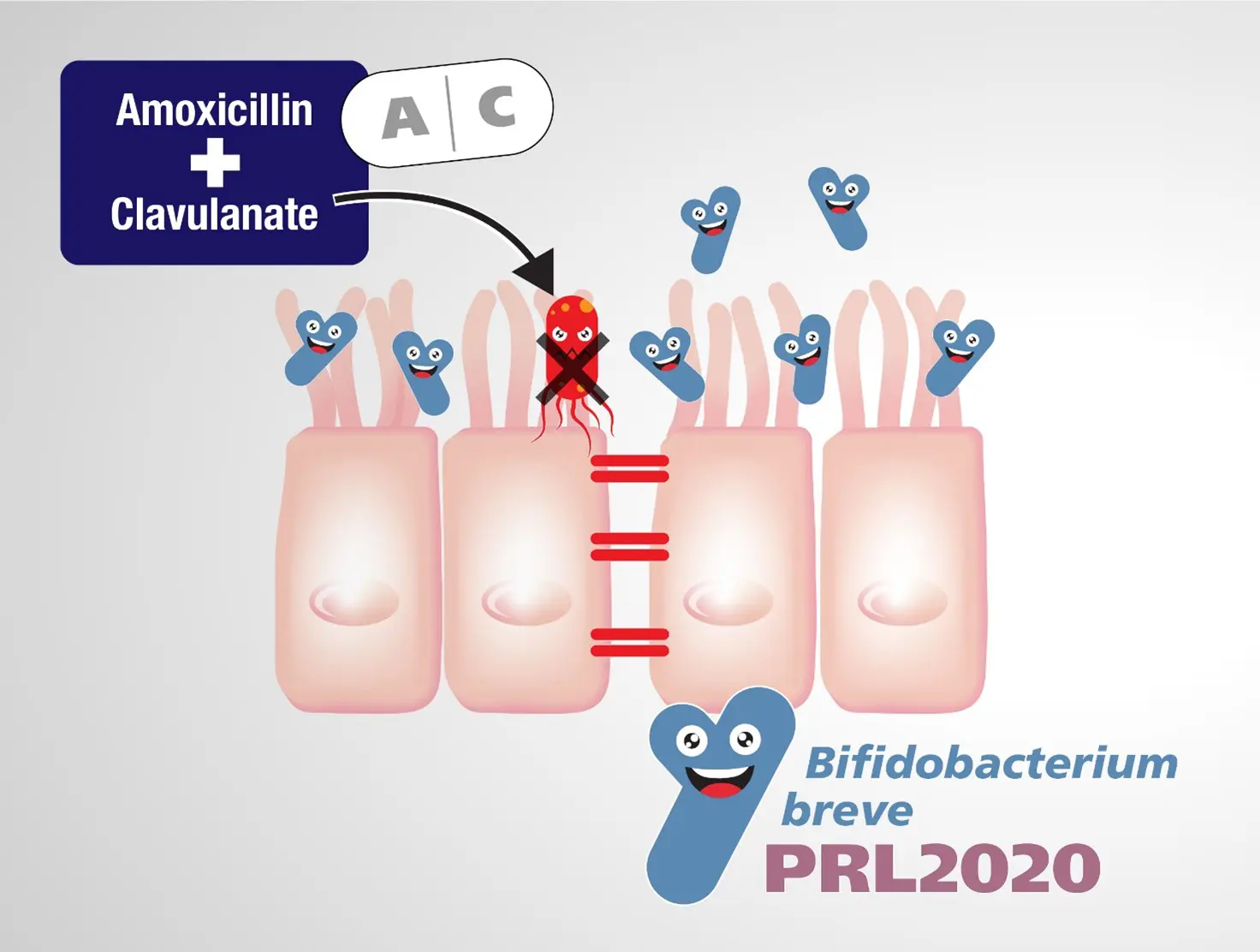
Amoxicillin + clavulanic acid (AMC) is one of the most frequently prescribed antibiotics in the Western world. It is a broad spectrum antibiotic and as such is capable of killing both Gram-positive and Gram-negative bacteria. A 2021 study by a group of Italian researchers engaged in the study of microbial genomics* specifically investigated the impact of this antibiotic formulation on the intestinal microbiota, noting a drastic reduction of bacteria in children treated with amoxicillin + clavulanic acid compared to the control group, resulting in a halving of the total content of bifidobacteria, a bacterial population of significant importance for human well-being.
This scenario has stimulated the search for a bifidobacterial strain that is able to resist AMC to investigate the possibility of its use as a probiotic to be taken in conjunction with this antibiotic therapy to repopulate the microbiota early.
The research group then performed appropriate experiments to probe the minimum inhibitory concentration of amoxicillin + clavulanic acid (MICAMC) for different bifidobacterial strains, some belonging to a collection of known strains and others isolated from children treated with AMC within the same collection. research. The determination of the susceptibility/resistance of these gut bifidobacteria strains showed that 98.5% of them are sensitive to AMC.
Only very few strains have been shown to be able to resist AMC, among these the Bifidobacterium breve PRL2020 showed the highest resistance value.
Simulating experiments on the intestinal microbiota showed that the PRL2020 strain is able to survive in the presence of a complex microbiota combined with the antibiotic AMC.
As a next step, the total safety of this bacterial strain was confirmed, also ascertaining its inability to transfer this peculiar resistance to other bacteria. which would reduce the effectiveness of antibiotic therapy.
These results supported the thesis concerning the ability of B. breve PRL2020 to grow in the presence of amoxicillin + clavulanic acid with the benefit of repopulating the intestinal microbiota of beneficial bifidobacteria making this strain an interesting candidate for the development of a new probiotic product to be used when AMC therapy is prescribed and prevent the dramatic decline in bifidobacteria that this usually involves.
* Mancabelli L, Mancino W, Lugli GA, Argentini C, Longhi G, Milani C, Viappiani A, Anzalone R, Bernasconi S, van Sinderen D, Ventura M, Turroni F. Amoxicillin-Clavulanic Acid Resistance in the Genus Bifidobacterium. Appl Environ Microbiol. 2021 Mar 11;87(7):e03137-20. doi: 10.1128/AEM.03137-20. PMID: 33483308; PMCID: PMC8091617.
